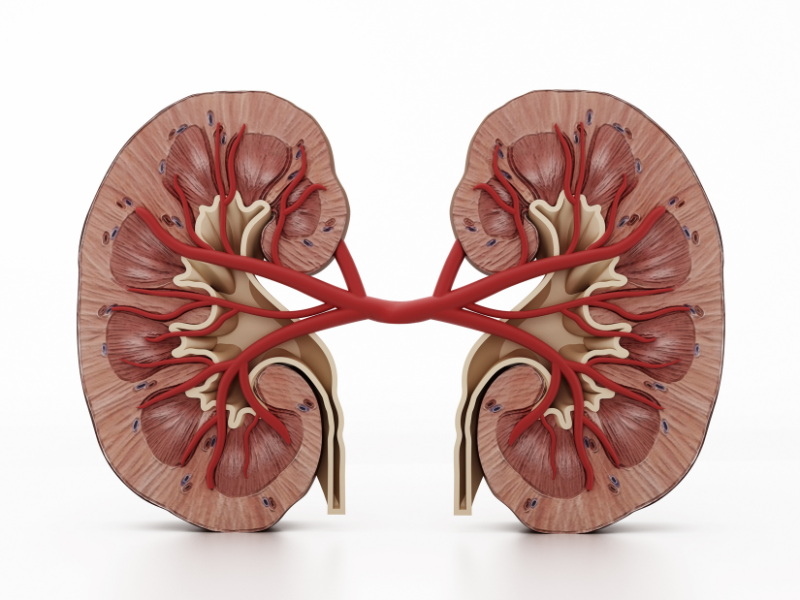
Acute Kidney Disease (AKI)
Acute kidney injury (AKI) is an abrupt decline in kidney function. It is a decline in the function of the kidney secondary to functional or structural changes to the kidney. It is measured by the increase markers in the blood called BUN & creatinine. For instance, AKI can occur because of kidney stones or mass, which causes obstruction of fluid from the kidney to the bladder. Other instances, AKI can be induced by drug toxicity. AKI can occur in patients with history of chronic kidney disease or no history of kidney disease at all. The role of the nephrologist is to identify the cause of the kidney injury and treat it. Early treatment is important in reversing the injury, and in some instances the injury can be permanent. In some cases, patients require renal replacement therapy such as hemodialysis because they are unable to remove toxins or excess fluid due to the extensive damage to the kidneys temporarily or permanently.
Chronic Kidney Disease (CKD)
Chronic kidney disease (CKD) is defined as decline in kidney function lasting longer than 3 months. There are five stages of CKD as described below. CKD can be diagnosed without knowledge of its cause. However, your doctor will order tests to help determine the cause. CKD is measured by a series of tests such as: elevation of the markers BUN & creatinine in the blood, abnormalities in urine sediment and chemistries, and abnormal finding on imaging studies. For example, hydronephrosis (fluid around the kidneys), polycystic kidney disease (multiple cysts on the kidneys), and small echogenic kidneys can be diagnosed by ultrasound, CT scans or MRI. Also, a person’s co-morbidities, such as hypertension or diabetes mellitus can predispose a patient to chronic kidney disease. Genetics can also predispose a patient to CKD. CKD is irreversible, and it will progress throughout a person’s life time. The overall goal of managing CKD is to slow the progression of kidney disease, and preserve the kidney function.
Different stages of CKD
Stage I: Kidney function of 90% and above
Stage II: Kidney function of 60-89%
Stage III: Kidney function of 30-59%
Stage IV: Kidney function of 15-29%
Stage V (ESRD): Kidney function of 14% or less
What are some risk factors for kidney disease progression?
- High blood pressure
- Diabetes Mellitus (type I and type II)
- African American race
- Male gender
- Obesity
- High cholesterol
- Smoking
- High-protein diet
- High protein level in the urine (greater than 1.5 grams/24 hour)
What can be done to reduce your risks of Kidney disease?
- Heart or kidney healthy diet
- Reduce sodium intake to 2 grams/day
- Tight glucose control, maintain a hemoglobin A1c level to less than 7.0
- Maintain good blood pressure control, blood pressure goal of less than 130/80
- Exercise daily
- Quit smoking
- Reduce protein intake to 80 grams/day
- Reduce total cholesterol to less than 200 and LDL to less than 100
- Discuss your overall health status with your physician for recommendations to how to improve your health and reduce your risk factors for kidney disease progression. Your doctor will give you specific recommendation for your specific condition.